This page as a pdf file
Wearing a continuous glucose sensor
John Davis talks about how he used a continuous glucose sensor. See the results, and the extraordinary things that his blood glucose did!
All blood glucose values are in US units - mg/dL. To convert to UK units - mmol/L - divide by 20 (knock off a nought and divide by two), or use our online BG unit converter.
Click on any chart to see it in more detail.
Introduction
Picture of MiniMed Continuous Glucose Monitoring System

The Continuous Glucose Monitoring System (CGMS) will automatically monitor glucose levels in your subcutaneous tissue located just underneath your skin. Glucose values from 40 (2.2) to 400 (22.2) are measured once every 5 minutes. Up to 288 values can be measured each day. Usually, you wear the CGMS for a maximum of three days.
The CGMS collects and stores all glucose values in its memory. Glucose values outside of the limits are recorded as if they were the limit. i.e. a value of 25.0 will be recorded as 22.2.
You have to take a minimum of 4 BG tests every day and enter them into the sensor. You also have to enter important events such as meals, insulin, exercise and any others that you establish with your hospital.
After 3-4 days you return to the hospital where the information is downloaded into the hospital computer. The computer will print a report of the daily glucose profiles. This information and your BG values, together with the other data, identifies patterns in your glucose levels and is used for better management of your diabetes.
The sensor does not have a screen which shows you your BG. You have to get it downloaded at the hospital.
My second experience with the sensor started on Friday 21 July.
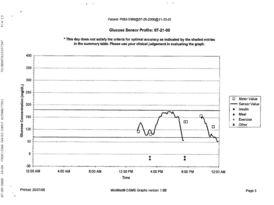
Friday 21 July 2000
Graph of Friday's glucose sensor results
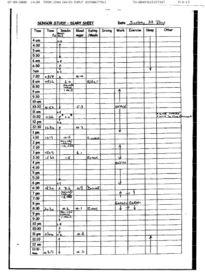
Friday's log sheet
[ Make log sheet bigger | view as text ]
Day 1
I duly reported to The Royal Bournemouth Hospital and was fitted with the sensor at 1.30pm. Unfortunately, after calibration it lost its way and had to be re-calibrated. (Involving another sensor at a cost of about £50). All was well with the second one and off I trolled home. Sensor in one pocket, the pump in the other.
7.30pm time for dinner. Took out the sensor to enter my data, and somehow unplugged the thing!! Put it back together again and reset it. You will notice from the graph the break in data. And so to bed, at 11.15pm my BG was 6.3. Normal for me, so I did nothing just went to sleep.
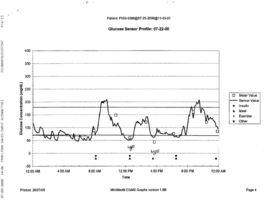
Saturday 22 July 2000
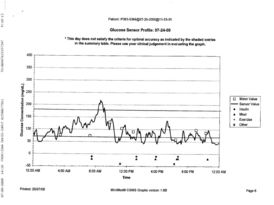
Graph of Saturday glucose sensor results
[ See graph bigger ]
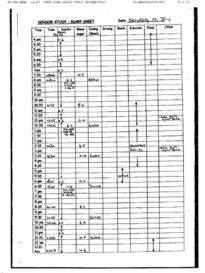
Saturday log sheet
[ See log sheet bigger | view as text ]
Day 2
7.30am Checked BG, 4.9. If you look at the graph you will clearly see that I was going hypo most of the night. Had breakfast, (65 CHO) checked BG at 10.30am, 8.2. At the time I thought O.K. but if you look on the graph it shows I had been up to around 12.0 earlier and was now on the way down. (Interesting?)
The rest of the day was spent on various household repairs and improvements, we have just moved house. Had a few slight hypos because I did not turn the pump off, or reduce the basal rate. I get plenty of warning signs and can take remedial action without doing so. And so to bed. BG at 11.50pm, 4.7. (a bit low.) 2 Rich Tea biscuits. Woke up at 2.27am, checked BG, 4.6. O.K. However, again you can clearly see from the graph that I was hypo before waking at 2.27am, had gone up to about 6.0, and had then dropped down again to about 2.7. Blissfully unaware, I slept on!
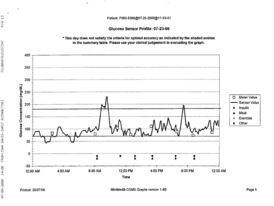
Sunday 23 July 2000
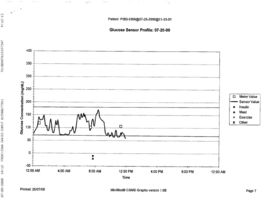
Graph of Sunday glucose sensor results
[ See graph bigger ]
Sunday log sheet
[ See log sheet bigger | view as text ]
Day 3
Woke at 8.00am BG, 4.4. Not bad considering I went to bed at 4.7.
Three hours later 5.3. But look at the graph!!! Up to about 13.0 at 10.30am. The rest of the day was uneventful, mostly spent on INPUT stuff, no hypos or hypers as the graph clearly shows. Bed at 12.30am BG, 6.5. No worries! But again, as you can see from the graph, nocturnal hypos gradually rising towards morning.
Monday 24 July 2000
Graph of Monday glucose sensor results
[ See graph bigger ]
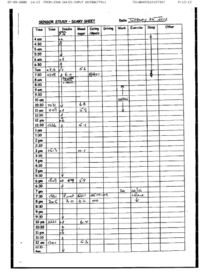
Monday log sheet
[ See log sheet bigger | view as text ]
Day 4
Up at 7.10am BG, 4.1. Another night with nocturnal hypos, again I was blissfully unaware! Rest of the day, normal apart from slight hypo at 6.17pm, 3.2. Bed at 12.30am, BG 6.5.
Tuesday 25 July 2000
Graph of Tuesday glucose sensor results
[ See graph bigger ]
Tuesday log sheet
[ See log sheet bigger | view as text ]
Day 5
Had a good night, no hypos. Sensor goes back lunchtime, I'll be sorry to see it go, I've only just got used to untangling the pump and sensor in the mornings, are they in love!
Conclusions
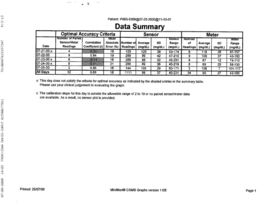
Table of summary data
[ See table bigger | view as text ]
At first having to wear a sensor and pump at the same time is a problem. The pump on one side of your body, the sensor on the other. It is not, in my opinion practical to wear them on the same side.
What do you do with them at night? Personally, I put both of them under the pillow and let them sort themselves out. Sometimes they got a bit tangled but it was never a problem.
The advantages to me were that knowing what my BG was doing every 5 minutes of the day enabled me to fine tune my basal rates. I have just done three days fasting, prior to my hospital check up. The results were amazing. Having been on the sensor and having adjusted my basals accordingly, has meant that no matter what the starting point was at the beginning. It remained there throughout the fasting period. This was true for the morning and afternoon fast, although I still needed to adjust my evening basal slightly, down to 0.6 from 0.8.
The two sessions I have had on the sensor has proved to me that BG levels swing up and down every minute and even testing every 2 hours with good results, does not mean that your BG is level between tests. Just look at the charts and compare them with my BG test times.
If you get the opportunity to go on the sensor, grab it with both hands! Wearing and using an insulin pump is a tremendous advance from multiple injections. But if you use the results of the Glucose Sensor to fine tune the pump, your control becomes even greater. Before I used the sensor I was hitting my target BG 84% of the time. Since using the sensor I now hit my numbers around 92% of the time!
Try it if you can!
John Davis
INPUT
See also:
Created: 7 Sep 2000; Last updated: Friday 25 January 2002
Other pages about food
[ What is a square-wave bolus? | Rewriting the diabetes rulebook | Calculating carbohydrates for recipes | Wearing a continuous glucose sensor | Books to help with diabetes ]
Other pages about blood testing
[ Wearing a continuous glucose sensor | My CGMS test | CGMS accuracy | Continuous Glucose Monitoring System | Cygnus GlucoWatch | Hypo review ]
Reader comments
-
On 2 Jun 2006 Christina wrote:
Great info
-
On 19 Jan 2001 Gary Lester wrote:
Hello Thanks for write up from John Davis. Has anyone done a 'Which'-type evaluation on pumps and testers now there are a few on the market. Who sells pumps and testers in the UK? Thanks Gary
-
On 21 Jan 2001 John Neale wrote:
John - if you look on our pump page you'll see there are 2 pump manufacturers in the UK. They will each let you try their pump for a month before you have to pay, so you can make up your own mind! For blood testers, there's a great review of all the meters at the Diabetes123 website.
-